A new sensitive technique can detect colorectal cancer in tissue samples—a method that could one day be used in clinical settings for early diagnosis.
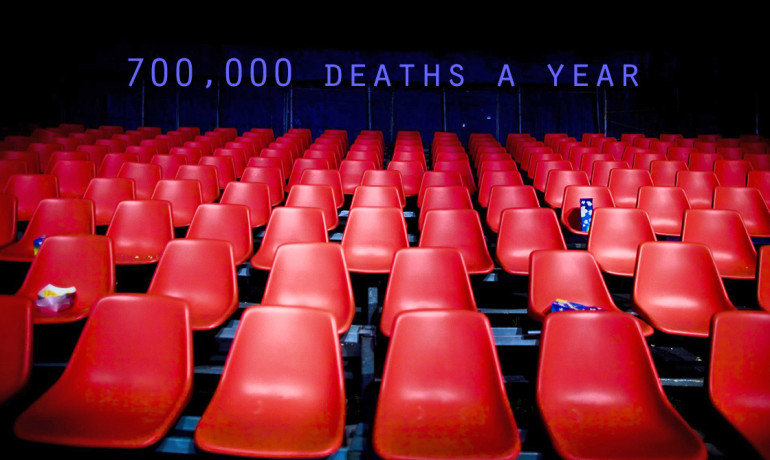
Late detection is one of the reasons the disease is so deadly, killing about 700,000 people every year.
“Currently, the average biopsy size required for a colorectal biopsy is about 300 milligrams,” says Ariel Furst, a graduate student at the California Institute of Technology (Caltech). “With our experimental setup, we require only about 500 micrograms of tissue, which could be taken with a syringe biopsy versus a punch biopsy. So it would be much less invasive.”
WHEN THINGS GO HAYWIRE
The researchers zeroed in on the activity of a protein called DNMT1 as a possible indicator of a cancerous transformation. DNMT1 is an enzyme responsible for DNA methylation—the addition of a methyl group to one of DNA’s bases.
This essential and normal process is a genetic editing technique that primarily turns genes off but that has also recently been identified as an early indicator of cancer, especially the development of tumors, if the process goes awry.
When all is working well, DNMT1 maintains the normal methylation pattern set in the embryonic stages, copying that pattern from the parent DNA strand to the daughter strand. But sometimes DNMT1 goes haywire, and methylation goes into overdrive, causing what is called hypermethylation.
Hypermethylation can lead to the repression of genes that typically do beneficial things, like suppress the growth of tumors or express proteins that repair damaged DNA, and that, in turn, can lead to cancer.
Furst and Jacqueline K. Barton, a chemistry professor at Caltech, devised an electrochemical platform to measure the activity of DNMT1 in crude tissue samples—those that contain all of the material from a tissue, not just DNA or RNA, for example.
Fundamentally, the design of this platform is based on the concept of DNA-mediated charge transport—the idea that DNA can behave like a wire, allowing electrons to flow through it and that the conductivity of that DNA wire is extremely sensitive to mistakes in the DNA itself. It can be used not only to locate DNA mutations but also to detect the presence of proteins such as DNMT1 that bind to DNA.
HOW THE NEW TECHNIQUE WORKS
In the present study, Furst and Barton started with two arrays of gold electrodes—one atop the other—embedded in Teflon blocks and separated by a thin spacer that formed a well for solution. They attached strands of DNA to the lower electrodes, then added the broken-down contents of a tissue sample to the solution well.
After allowing time for any DNMT1 in the tissue sample to methylate the DNA, they added a restriction enzyme that severed the DNA if no methylation had occurred—in other words, if DNMT1 was inactive. When they applied a current to the lower electrodes, the samples with DNMT1 activity passed the current clear through to the upper electrodes, where the activity could be measured.
“No methylation means cutting, which means the signal turns off,” explains Furst. “If the DNMT1 is active, the signal remains on. So we call this a signal-on assay for methylation activity. But beyond on or off, it also allows us to measure the amount of activity.”
Using the new setup, the researchers measured DNMT1 activity in 10 pairs of human tissue samples, each composed of a colorectal tumor sample and an adjacent healthy tissue from the same patient. When they compared the samples within each pair, they consistently found significantly higher DNMT1 activity, hypermethylation, in the tumorous tissue.
Notably, they found little correlation between the amount of DNMT1 in the samples and the presence of cancer—the correlation was with activity.
“The assay provides a reliable and sensitive measure of hypermethylation,” says Barton. “It looks like hypermethylation is good indicator of tumorigenesis, so this technique could provide a useful route to early detection of cancer when hypermethylation is involved.”
Looking to the future, Barton’s group hopes to use the same general approach in devising assays for other DNA-binding proteins and possibly using the sensitivity of their electrochemical devices to measure protein activities in single cells.
Such a platform might even open up the possibility of inexpensive, portable tests that could be used in the home to catch colorectal cancer in its earliest, most treatable stages.
The National Institutes of Health supported the research, which is described in a study published in the journal Chemistry & Biology.
Fuente: www.futurity.org
WARNING: Virgnia T Sherl made this note and was not rated by users as credible.